VersaWrap® is a medical device implant that provides a gliding surface for tendons and peripheral nerve in hand, wrist, elbow, and other upper extremity procedures
- Tenolysis
- Zones 2-5, TI -TIII (flexor)
- Zones 3-8, TII -TV (extensor)
- Neurolysis (redo carpal, cubital)
- Nerve trauma
- Tendon trauma
- Tendon or nerve transfers
Examples of VersaWrap application in upper extremity procedures
Click the images to learn more
FPL repair second look
-
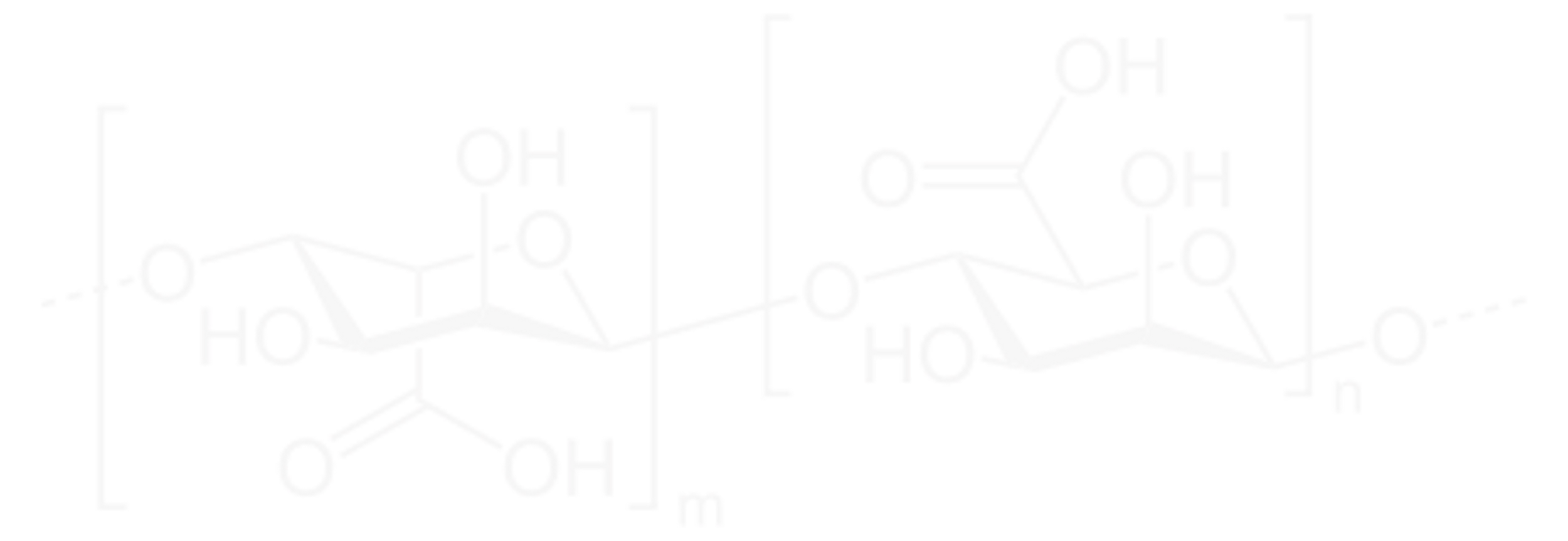
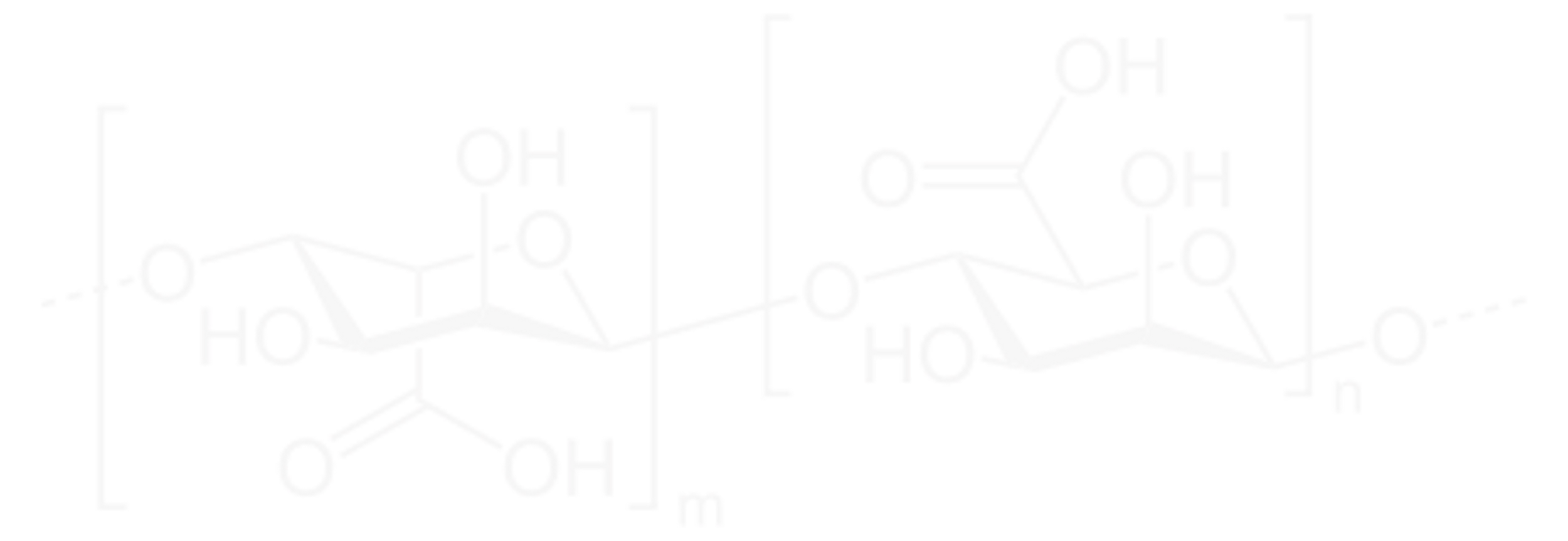
A 68-year-old patient sustained an acute flexor pollicis longus (FPL) tendon laceration when he fell on glass, cutting his right wrist. During the operative repair VersaWrap (a hyaluronic acid(HA)/alginate sheet with activating solution) was applied over the repair site to limit unwanted postoperative tethering.
before undergoing distal radius fracture operative fixation for a separate injury one year later, allowing direct visualization of the healed tendon repair.
-
At his final follow up appointment (10 weeks postop), he was able to make a full composite fist and had 30 degrees of flexion about the right thumb IPJ when compared to 45 degrees on the contralateral extremity. He had resumed normal activity and was cleared without restrictions.
-
Approximately one year later, the patient sustained a right distal radius fracture after falling off a ladder and underwent a right distal radius open reduction and internal fixation. The exposure revealed the previously repaired FPL, which was intact. The repair was visualized and noted to have healed entirely. There were no adhesions in the area where VersaWrap had been applied. Proximal to the placement of VersaWrap, though, adhesions were noted.
Recurrent cubital tunnel release
-
A 68-year-old male with a history of two previous cubital tunnel releases who presented with persistent symptoms related to ulnar nerve compression at the elbow.
-
Patient underwent repeat cubital tunnel release with submuscular transposition of the ulnar nerve. VersaWrap was used to wrap the ulnar nerve to reduce postoperative scarring
-
The surgeon stated that VersaWrap protected the nerve from tethering to surrounding tissues. At six (6) weeks follow-up, the patient was improved with positive postoperative outcomes.
Migraine case
-
Chronic intractable migraine headaches
-
A 63-year-old female who presented with chronic intractable migraine headaches originating from the occipital trigger site. The headaches persisted previously for thirty (30)years. The patient had up to eight (8) episodes of severe headaches every month that would last days to weeks. The headaches did not get better with medication, radiofrequency ablation, nerve blocks, and Botox injections. The patient underwent decompression and neurolysis of bilateral greater occipital nerves. VersaWrap was used to wrap the nerves to reduce postoperative scarring
-
At one-month follow-up, the patient has only had one mild self-limiting headache and is otherwise headache free. VersaWrap served as a barrier and nerve protector to reduce scarring with good postoperative outcomes.
-
The patient is a 73-year-old male who was walking a dog when the dog leash yanked suddenly, causing immediate pain in the patient’s dominant right hand.
Pre-operative assessment revealed the patient had a swollen and slightly bruised small finger with absent FDP function. Sensation was present throughout all fingers.
Surgical exploration was conducted at 26 days post-injury and the small finger FDP was found ruptured in the palm, at the transverse carpal ligament level. A small organized hematoma was found in the palm, around the common digital nerves to the small finger.
-
Red arrow is edge of transverse carpal ligament, opened to allow access to tendon in canal; black arrow is tendon repair site; blue arrow is nerve and vessel crossing over tendon (hematoma has already been washed away).
The small finger FDP was repaired and neurolysis of the digital nerves to the small finger was conducted, debriding the hematoma.
VersaWrap was wrapped around the tenorrhaphy site and digital nerves where neurolysis was conducted.
Post-operatively a routine flexor tendon rehabilitation protocol was followed along with supervised hand therapy.
-
At five months follow-up, the patient has excellent active motion. The patient makes a full composite fist with no flexion contractures. The soft tissue envelope is in excellent condition with normal sensation in the digital nerves to the injured small finger.
Ruptured FDP with a hematoma around common digital nerves
Laceration of FDP, FDS, and digital nerve of the small and ring fingers
-
The patient is a 34-year-old active male who sustained a volar aspect laceration across the small finger at the DIP joint level and across the ring finger at the PIP joint level from a spinning piece of sheet metal.
He experienced numbness along the ulnar border of both the small and ring fingers, and absent FDP tendon function to both the small and ring fingers.
Surgical exploration was performed at 9 days post-injury. The small finger FDP and ring finger FDP were both found to be lacerated. One of the two slips of the ring finger flexor digitorum superficialis (FDS) was also lacerated. The ulnar digital nerves of both fingers were also lacerated.
-
FDP of both small and ring fingers were repaired. The FDS of the ring finger was repaired.
VersaWrap was placed around the repaired tendons and nerves to allow tissue gliding.
Post-operatively a routine flexor tendon rehabilitation protocol was followed.
-
At three months follow-up, the patient has excellent range of motion of all digits. The scars are remodeling very well with excellent soft tissue envelopes in both digits. The patient shows independent glide between FDS and FDP with mild residual stiffness. Tinel’s sign over the repaired digital nerves is out to the DIP flexion crease level.
Laceration of FDP and FDS with contused common digital nerves
-
The patient is a 23-year-old male who sustained an accidental self-inflicted knife wound to the right, dominant hand.
Patient presented with absent sensation along ulnar border of small finger and absent flexor tendon function to the small finger.
Surgical exploration was performed at 17 days post-injury. The small finger FDP and FDS were found to be lacerated. The digital nerves of the small finger had contusions but were not completely lacerated.
-
The small finger FDP and both slips of FDS were repaired. Each tenorrhaphy site was treated with VersaWrap.
Post-operatively a routine flexor tendon rehabilitation protocol was followed along with supervised hand therapy.
-
At three months follow-up, the patient has excellent range of motion of all digits. The patient made a full composite fist with no flexion contractures. The soft tissue envelope is in excellent condition with normal sensation in the digital nerves to the injured small finger.
Sensation is equal in all digits with a 5 mm 2-point discrimination, including the small finger with the nerve contusion.
Thumb flexor tendon tenolysis with ulnar and radial nerve repair
-
The patient is a 23-year-old female who sustained an accidental self-inflicted broken bottle wound to the right, dominant hand.
Patient presented with thumb numbness and absent flexor pollicis longus tendon function to the thumb.
Surgical exploration was performed at 36 days post-injury; both digital nerves in the thumb were found to be lacerated and the FPL was partially injured.
-
Microscope assisted repair of both digital nerves was conducted along with tenolysis of the injured FPL.
VersaWrap was wrapped around the repaired tissues to minimize tethering.
Standard rehabilitation for nerve and tendon injuries with supervised care from a certified hand therapist was initiated at 10 days postop.
-
At twelve months follow-up the patient had excellent recovery including full range of motion.
The patient presented no signs of tendon or nerve tethering or adhesions. Nerve recovery was good and continued to improve.
Sensation was consistently improving over time with an 8 mm 2-point discrimination of both radial and ulnar digital nerves in the thumb. There was no paresthesiae.
Breast reconstruction
-
Breast reconstruction with abdominal-based free flap and transfer of intercostal sensory nerves into abdominal cutaneous nerve branches. Breast reconstruction improves a woman’s self-image and restores a sense of normality following mastectomy. When conducted with tissues from the abdomen, nerves from the chest wall can be transferred into nerves in the abdomen to restore some sensation in the breast. Typically, long nerve grafts are required for this procedure. Outcomes have previously been hampered by these long grafts. Using VersaWrap as a guide during flap inset allows for use of shorter nerve grafts, protects the repair site, and may help prevent tethering of the nerve coaptation during flap movement
-
A 60-year-old woman with bilateral ductal carcinoma in situ who underwent bilateral skin sparing mastectomies. She had bilateral deep inferior epigastric perforator (DIEP breast reconstruction) with transfer of one intercostal nerve into one abdominal cutaneous nerve on each side. One (1) 2 x 2 in VersaWrap was cut in half into two (2) 1 x 2 in pieces. The VersaWrap pieces were shaped into a funnel using the accompanying paper backing. The VersaWrap funnels allowed the abdominal cutaneous nerves to be coapted to a 3cm graft during flap inset, on each side. Once the nerves were together, the VersaWrap paper backing was removed and the VersaWrap sheet adhered to the nerve coaptions, supporting the repair. Without VersaWrap, the graft would have been 6-7cm for proper visualization. On postoperative Day 4 the patient was discharged from the hospital with healed incisions and she is very happy with the appearance of her breasts two (2) months after surgery. She has returned to gardening and walking daily at two months. Sensation has not returned to her flap tissues yet but is not expected before 3-6 months.
-
A 41-year-old woman with invasive ductal carcinoma of the right breast who has had bilateral mastectomies. She had bilateral deep inferior epigastric perforator (DIEP breast reconstruction) with transfer of one intercostal nerve into one abdominal cutaneous nerve on each side. One (1) 2 x 2 in VersaWrap was cut half into two (2) 1 x 2 in pieces. VersaWrap pieces were applied to each side, allowing coaptation of the intercostal nerve to the abdominal cutaneous nerve through a 3cm (right), and 6 cm (left) nerve graft. The patient was discharged on postoperative Day 4 in good condition. Incisions are healed and she is very happy with the appearance of her breasts two (2) months after surgery. She has returned to playing basketball with her children and to doing yoga. Sensation has not returned to her flap tissues yet but is not expected before 3-6 months.
-
This patient is a 69-year-old female with a history of numerous previous breast surgeries, right breast cancer treated 20 years prior with lumpectomy, implant placement, and radiation. She now has a capsular contracture and breast asymmetry. She is otherwise healthy. She had a complete capsulectomy with implant removal, replaced with a free superficial inferior epigastric perforator flap (SIEA) from the left lower abdomen. At the time of flap surgery, one intercostal nerve was transferred into two abdominal perforator nerves through a 5cm graft. One (1) 2 x 2 in VersaWrap was cut half into two (2) 1 x 2 in pieces. A single VersaWrap piece was applied to the right breast in the same manner as the previous cases, allowing coaptation of the intercostal nerve to the abdominal perforator nerves.
Patient 3 developed a hematoma on postoperative Day 3 and was taken back to the OR for hematoma evacuation. The nerve repair was visualized and noted to be intact. The applied VersaWrap was visualized, remaining wrapped around the nerve where implanted. VersaWrap isolated the nerve repair, preventing the repair from adhering to the underlying pectoralis major muscle. The patient was discharged home on postoperative Day 5 in good condition. She had a superficial surgical site infection in the right breast on postoperative Day 7 that resolved with a 5-day course of doxycycline. She is doing well and happy with the appearance of her breast 1.5 months after surgery. Sensation has not returned to her flap tissues yet but is not expected before 3-6 months.
-
This patient is a 34-year-old woman with a BRCA-1 gene mutation at high risk for breast cancer who underwent bilateral nipple sparing mastectomies. She had bilateral deep inferior epigastric perforator (DIEP breast reconstruction) with transfer of one intercostal nerve into one abdominal cutaneous nerve on each side. One (1) 2 x 2 in VersaWrap Tendon Protector was cut half into two (2) 1 x 2 in pieces. VersaWrap pieces were applied to each side in the same manner as the previous cases, allowing coaptation of the intercostal nerve to the abdominal cutaneous nerve through a 4cm (right), and 3 cm (left) nerve graft.
The patient was discharged home on postoperative Day 3 in good condition. She is back to most of her normal activities one (1) month after surgery and is happy with the appearance of her breasts. Sensation has not returned to her flap tissues yet but is not expected before 3-6 months.
-
In these four cases, the VersaWrap allowed for use of shorter nerve grafts, which is expected to improve the recovery of sensation within the abdominal tissue flaps. Each patient is doing well after surgery with no known complications or side effects associated with the use of VersaWrap for nerve coaptation. Case 3 demonstrates that the VersaWrap remains present around the nerve three (3) days postoperative and was observed to prevent adhesion of the nerve coaptation to surrounding tissues. Sensory recovery is not expected for several more months in any of these patients.